|
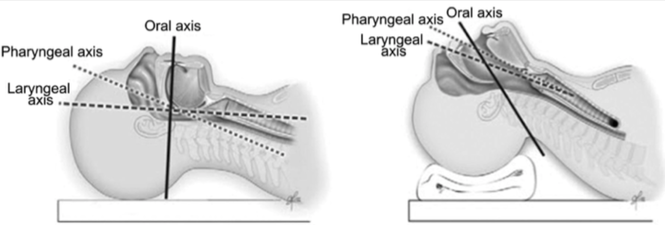
By Perry Lee, MD (PGY-3) Advanced airway management is a mainstay of an emergency physician’s armamentarium. Many practitioners establish a routine with personal nuances established either by their training or from prior experiences. Here we examine common techniques and their effectiveness. The studies selected are not meant to drastically change your systematic practice, but give recognition to the variability in routine that can still achieve a successful intubation. In addition to technique, intubation success also relies on muscle memory from repetitive practice, operator confidence from successful mental visualization, and the ability to calmly troubleshoot a difficult airway. 1. SNIFFING POSITIONING Optimal positioning of the head and neck should allow for improved laryngeal visualization during direct laryngoscopy (DL) and should therefore increase first intubation success. A 2015 meta-analysis of randomized controlled trials (RCT) concluded that the sniffing position (alanto-occipital extension with head elevation) despite showing NO improvement in glottis visualization, first intubation success, or intubation time compared to a simple head extension position, should still be used as the standard head positioning as it provides easier intubation conditions.[i] 2. VIDEO LARYNGOSCOPY Video laryngoscopy (VL) is increasingly being used as a first attempt adjunct when intubating with multiple studies showing improved success when VL is used.[ii][iii][iv][v][vi] However, a 2017 RCT meta-analysis for patients in the emergency department (ED), intensive care unit (ICU), and prehospital settings requiring tracheal intubation showed NO improved first-attempt success when using video laryngoscopy compared to direct laryngoscopy.[vii] In fact it shows that prehospital intubation success was worse when experienced operators used video laryngoscopy. 3. BOUGIE The gum-elastic bougie is a semi-flexible device that allows a seldinger-like technique to intubate a patient. Rather than a routine device, most physicians use the bougie as a rescue device after a failed intubation attempt. A SINGLE CENTER RCT study published in 2018 using the bougie as a primary intubation device showed first-pass success greater with bougie use versus endotracheal tube (ETT) and stylet use (98% vs 87%).[viii] 4. BURP Improved glottis visualization by backward, upward, and rightward pressure (BURP) on the thyroid cartilage to displace the larynx has been noted in multiple observational studies.[ix][x][xi]w [i]Akihisa Y, Hoshijima H, Maruyama K, Koyama Y, Andoh T. Effects of sniffing position for tracheal intubation: a meta-analysis of randomized controlled trials. Am J Emerg Med. 2015 Nov;33(11):1606-11. [ii]Mosier, JM, Stolz, U, Chiu, S, and Sakles, JC. Difficult airway management in the emergency department: GlideScope videolaryngoscopy compared to direct laryngoscopy. J Emerg Med. 2012; 42: 629–634 [iii]Sakles, JC, Mosier, JM, Chiu, S, and Keim, SM. Tracheal intubation in the emergency department: a comparison of GlideScope(R) video laryngoscopy to direct laryngoscopy in 822 intubations. J Emerg Med. 2012; 42: 400–405 [iv]Michailidou, M, O’Keeffe, T, Mosier, JM et al. A comparison of video laryngoscopy to direct laryngoscopy for the emergency intubation of trauma patients. World J Surg. 2015; 39: 782–788 [v]Silverberg, MJ, Li, N, Acquah, SO, and Kory, PD. Comparison of video laryngoscopy versus direct laryngoscopy during urgent endotracheal intubation: a randomized controlled trial. Crit Care Med. 2015; 43: 636–641 [vi]Sakles, JC, Patanwala, AE, Mosier, JM, and Dicken, JM. Comparison of video laryngoscopy to direct laryngoscopy for intubation of patients with difficult airway characteristics in the emergency department. Intern Emerg Med. 2014; 9: 93–98 [vii]Abdelgadir IS, Phillips RS, Singh D, Moncreiff MP, Lumsden JL. Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates). Cochrane Database Syst Rev. 2017 May 24;5:CD011413. [viii]Driver BE, Prekker ME, Klein LR, Reardon RF, Miner JR, Fagerstrom ET, Cleghorn MR, McGill JW, Cole JB. Effect of Use of a Bougie vs Endotracheal Tube and Stylet on First-Attempt Intubation Success Among Patients With Difficult Airways Undergoing Emergency Intubation: A Randomized Clinical Trial. JAMA. 2018 Jun 5;319(21):2179-2189. [ix]Benumof JL, Cooper SD. Quantiative improvement in laryngoscopic view by optimal external laryngoscopic manipulation. Anesthesia and Analgesia Journal of Clinical Anaesthesia 1996;8:136-140. [x]Takahata O, Kubota M, Mamiya K et al. The efficacy of the Anesthesia and Analgesia 1997;84:419-421. [xi]Vanner RG, Clarke P, Moore WJ et al. The effect of cricoid pressure and neck support on the view at laryngoscopy. Anaesthesia 1997;52:896-900.
1 Comment
11/21/2022 08:37:16 pm
Thanks for the information l read your article l am very impressive
Reply
Leave a Reply. |
ABOUT USVegasFOAM is dedicated to sharing cutting edge learning with anyone, anywhere, anytime. We hope to inspire discussion, challenge dogma, and keep readers up to date on the latest in emergency medicine. This site is managed by the residents of Las Vegas’ Emergency Medicine Residency program and we are committed to promoting the FOAMed movement. Archives
June 2022
Categories |
CONTACT US901 Rancho Lane, Ste 135 Las Vegas, NV 89106 P: (702) 383-7885 F: (702) 366-8545 |
ABOUT US |
WHO WE ARE |
WHAT WE DO |
STUDENTS |
RESEARCH |
FOAM BLOG |
© COPYRIGHT 2015. ALL RIGHTS RESERVED.
LasVegasEMR.com is neither owned nor operated by the Kirk Kerkorian School or Medicine at UNLV . It is financed and managed independently by a group of emergency physicians. This website is not supported financially, technically, or otherwise by UNLVSOM nor by any other governmental entity. The affiliation with Kirk Kekorian School of Medicine at UNLV logo does not imply endorsement or approval of the content contained on these pages.
Icons made by Pixel perfect from www.flaticon.com
Icons made by Pixel perfect from www.flaticon.com

 RSS Feed
RSS Feed
