|
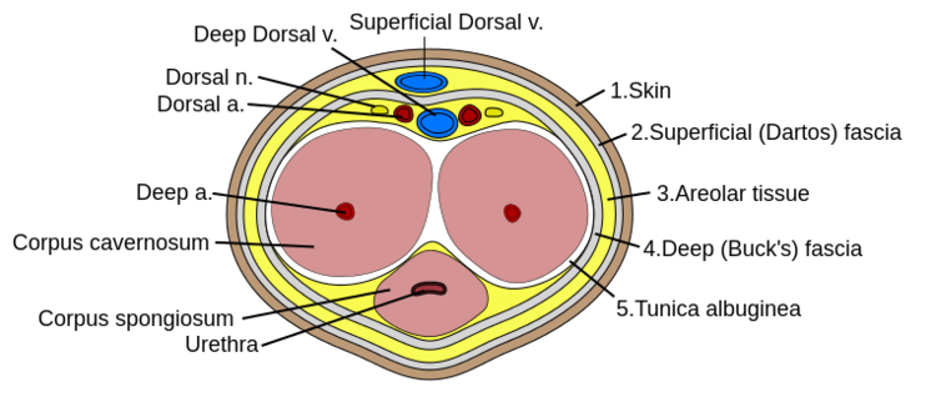
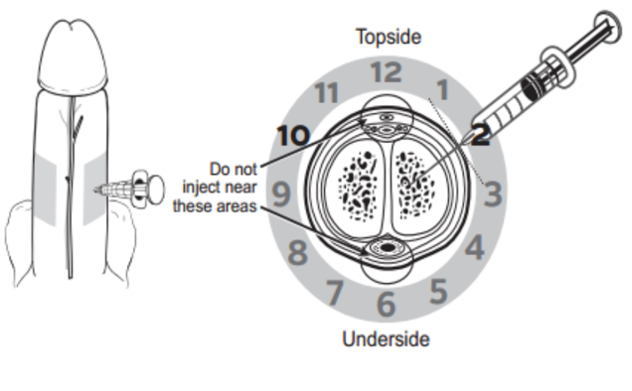
Author: Lisa Di Tomaso, DO PGY-3 Reviewed by: James Bailey, MD Introduction: Priapism is defined as a sustained erection lasting longer than 4 hours that is not associated with sexual stimulation. It can lead to penile necrosis and erectile dysfunction with the risk increasing after 24 hours. Between 2006 and 2009 approximately 32,000 visits were for priapism, an incidence of 5.3 per 100,000 males per year. The incidence increased by 31% during summer months, likely due to an increase in trauma which is a known cause. Pathophysiology: Before getting into the pathology of priapism, it’s important to review a little bit of anatomy. The corpus cavernosum are twin parallel structures that fill with blood to achieve an erection. The veins run on the dorsal aspect in the midline and the urethra, surrounded by corpus spongiosum, runs along the medial ventral aspect. There are two types of priapism, high-flow also called non-ischemic, and low flow or ischemic priapism. High-flow (non-ischemic) priapism is typically caused by injury either to the perineum with a straddle injury or to the spinal cord. High-flow priapism is usually painless and a blood sample from the corpus cavernosum will be arterial in appearance and on blood gas analysis. The assumed mechanism for a spinal cord injury is the abrupt loss of sympathetic output to pelvic vasculature leads to increased parasympathetic output and thus uncontrolled arterial flow into penis. Injuries to the perineum, usually a straddle type injury, can cause an arterio-cavernosal shunt leading to increased arterial inflow. Low-flow priapism is more common and is a urologic emergency as it can cause penile necrosis and erectile dysfunction. Unlike high-flow, it is painful and usually the shaft is hard while the glans is soft. It is caused by some sort of veno-occlusion which leads to pooling of deoxygenated blood in cavernosal tissues. The pooling of deoxygenated blood can prevent further arterial inflow leading to tissue ischemia and necrosis if not treated and sexual dysfunction if intervention is not performed in time. It can be caused by hematologic disorders such as leukemia or sickle cell disease, DIC, pelvic malignancy or drugs, both prescription and illicit. Common prescription triggers include anti-depressants particularly SSRI’s and trazadone, anti-psychotics and cocaine is a well-known trigger from illicit substances. It is also worth noting that erectile dysfunction medications like sildenafil (Viagra) can cause a priapism if the intended erection for sexual intercourse does not resolve after 4 hours. Management: The management depends on the type of priapism. High-flow (non-ischemic) priapism is managed by treating the underlying cause. It usually self-resolves without intervention and does not cause ischemia or sexual dysfunction. Low-flow (ischemic) priapism can be managed in a step-wise approach. Don’t forget pain control if needed for patient comfort or cooperation which can be achieved with narcotics or a penile nerve block. A penile nerve block is performed by local infiltration of anesthetic with a 27g needle at the base of the penis at the 2/3 o’clock and 9/10 o’clock positions or as a ring block to target the dorsal nerves. As the penile vasculature runs in the midline, be sure to aspirate before injecting and stay lateral to prevent an incidental intravenous injection of the anesthetic. The steps involved in management of low-flow priapism can be remembered as below: 1.Aspirate 25mL from cavernosum, 2x 2.Irrigate cavernosum with 25mL of cold saline 3.Medication injection 4.Wrap in elastic bandage after detumescent achieved 5.Consult if Refractory --> urology for shunt procedure Before choosing to aspirate be sure the patient is a candidate and would benefit. If the priapism has been present longer than 48 hours there is rare benefit and there is a high risk of impotence even with treatment. If your patient is an appropriate candidate then it is safe to proceed. Be sure to obtain informed consent and then prep the penis with chlorhexidine and drape appropriately. If a penile nerve block had not been previously performed, you could choose to do one now or inject local anesthetic at aspiration site. Similar to aspiration you will insert an 18g needle into the shaft at the 2/3 o’clock and 9/10 o’clock positions and aspirate about 20-30cc of blood from each side. If choosing to proceed to injection or irrigation, you can leave the needle in place at this step. For irrigation you will irrigate each side of the cavernosum with 20-30mL of cold saline. If detumescence has still not been achieved than you can proceed with medication injection. In adult patients the drug of choice is phenylephrine and epinephrine has been shown to be more effective in the pediatric population. You will first need to dilute 1mL of the phenylephrine 1mg/mL in a 9mL normal saline flush for a final concentration of 100mcg/mL. This is the same process as making a push-dose epinephrine. At a phenylephrine concentration of 100mcg/mL you will inject 100-200mcg (1-2mL) every 3-5 minutes with a maximum dosage of 1000mcg (10mL) until detumescence has been achieved or one hour has elapsed. Before injecting phenylephrine make sure the patient is on the cardiac monitor and watch for reflex bradycardia, use caution in patients with cardiovascular disease. Unlike aspiration you only need to inject one side as the channel between the cavernosa is sufficient to treat both sides. If all efforts have failed, you can try wrapping the penis in an elastic bandage or having the patient run in place or do squats.
If the patient has sickle cell disease treatment should also be aimed at treating the underlying cause with IV fluids, pain control and supplemental oxygen. You can also consider transfusion for a goal hematocrit of >30%. Disposition: Disposition depends on the underlying cause and success of treatment. If the priapism is high-flow the disposition will depend on the management of the underlying cause but will usually be admission for the inciting trauma. If the low-flow priapism was successfully treated in the emergency department and detumescence was achieved, then the patient can be safely discharged with outpatient urology follow-up. Be sure to give counseling on avoidance of using ED medications or illicit substances if this was found to be the cause. If all the above methods of management failed and the patient still has a priapism, then an emergent consult to urology is necessary for likely urology or interventional radiology intervention. References: Roghmann F, Becker A, Sammon JD, Ouerghi M, Sun M, Sukumar S, Djahangirian O, Zorn KC, Ghani KR, Gandaglia G, Menon M, Karakiewicz P, Noldus J, Trinh QD. Incidence of priapism in emergency departments in the United States. J Urol. 2013 Oct;190(4):1275-80. doi: 10.1016/j.juro.2013.03.118. Epub 2013 Apr 9. PMID: 23583536. Rosen's Emergency Medicine : Concepts and Clinical Practice. St. Louis :Mosby, 2002. Quarles A, Ogele E, Quigley M(2017, July 4). Priapism: The ED Focused Appropach. [NUEM Blog. Expert Commentary By Bennett N]. Retrieved from http://www.nuemblog.com/blog/priapism
0 Comments
Leave a Reply. |
ABOUT USVegasFOAM is dedicated to sharing cutting edge learning with anyone, anywhere, anytime. We hope to inspire discussion, challenge dogma, and keep readers up to date on the latest in emergency medicine. This site is managed by the residents of Las Vegas’ Emergency Medicine Residency program and we are committed to promoting the FOAMed movement. Archives
June 2022
Categories |
CONTACT US901 Rancho Lane, Ste 135 Las Vegas, NV 89106 P: (702) 383-7885 F: (702) 366-8545 |
ABOUT US |
WHO WE ARE |
WHAT WE DO |
STUDENTS |
RESEARCH |
FOAM BLOG |
© COPYRIGHT 2015. ALL RIGHTS RESERVED.
LasVegasEMR.com is neither owned nor operated by the Kirk Kerkorian School or Medicine at UNLV . It is financed and managed independently by a group of emergency physicians. This website is not supported financially, technically, or otherwise by UNLVSOM nor by any other governmental entity. The affiliation with Kirk Kekorian School of Medicine at UNLV logo does not imply endorsement or approval of the content contained on these pages.
Icons made by Pixel perfect from www.flaticon.com
Icons made by Pixel perfect from www.flaticon.com

 RSS Feed
RSS Feed
