|
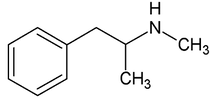
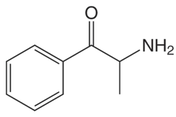
By: Weston Hampton, MD PGY3 Reviewed by: Eugene Kang, MD Over the past decade, a new drug has emerged across the world, medically known as cathinones but known to the public as bath salts. This is a large and heterogenous group of beta-ketone amphetamine analogs that gained popularity as an illicit substance around 2009. Many cathinones are naturally occurring, most commonly known as the substance Khat present in Catha edulis, a flowering plant most prominent in Eastern Africa that was frequently chewed by native communities for its euphoric effects. While structurally similar to methamphetamines, there are slight changes in the affected neuroendocrine pathways and duration of symptoms. As a group, cathinones stimulate both alpha- and beta-adrenergic receptors and inhibit reuptake of norepinephrine, dopamine, and serotonin. Reuptake inhibition can occur in different proportions depending on the type of cathinone used. Cathinones are generally lipophilic and readily cross the blood brain barrier accounting for their rapid onset of neuropsychiatric symptoms. Compared mechanistically to methamphetamines, the addition of a beta-ketone group in cathinones gives them relatively equal blockade of norepinephrine and dopamine reuptake, and are far less selective for serotonin when compared to methamphetamine.
Methamphetamine Cathinone (common phenylethylamine) (from khat) The earliest reported synthetic cathinone is methcathinone, created in the 1920’s and mass produced in the USSR as an antidepressant. These substances began to have widespread recreational use in 2009 in Europe, then in 2010 in the US. The term “bath salts” was a marketing tactic used to avoid various regulatory bodies during shipping. Synthetic cathinones as a group are heterogenous with at least 150 novel variations on the market, which lends to the difficulty in their detection through routine drug screens. Clinically, synthetic cathinones typically manifest with a sympathomimetic toxidrome with an overlying neuropsychiatric component with half-lives that are extremely variable, again due to the wide variance of chemical structures. These patients are at high risk for hyperthermia due to increase muscle activity and should have temperature monitored closely throughout the ED course. They are similarly at high risk for rhabdomyolysis, with one small study suggesting greater than one-fourth of synthetic cathinone ingestions leading to severe rhabdomyolysis. Treatment for these patients remains supportive. Benzodiazepines are recommended as first line agents. Antipsychotics should be given mindfully and with caution as they can lower the seizure threshold, prolong the QT interval, and reduce heat dissipation in these patients. In conclusion, synthetic cathinones are becoming more common as a drug of abuse and require a high index of suspicion. Intoxication with these substances remains a clinical diagnosis as they cannot reliably be detected on normal toxicological screens. Their heterogeneity as a group can give a wide variety of symptom severity and duration, and in general should be treated supportively. Recommendations: -Remain suspicious of synthetic cathinones in agitation/intoxication -Check temperature and use cooling techniques for hyperthermia, antipyretics are ineffective -Benzodiazepines are preferred choice for agitation -CK and renal function tests indicated due to increased likelihood of rhabdomyolysis References: Abouchedid and Wood. Cathinones. Clinical Toxicology and Emergency Medicine. 2017. Banks et al. Synthetic Cathinones and amphetamine analogues: What’s the rave about? J Emerg Med. Aug 2017 Gershman et al. Synthetic Cathinones (‘Bath Salts’) Legal and Health Care Challenges. Pharmacy and Therapeutics. Oct 2012. O’Connor et al. Prevalence of Rhabdomyolysis in Sympathomimetic Toxicity: a Comparison of Stimulants. Journal of Medical Toxicology. June 2015. Arnold and Ryan. Acute amphetamine and synthetic cathinone ("bath salt") intoxication. Uptodate. March 2021. De Felice et al. Synthetic cathinones: Chemical phylogeny, physiology, and neuropharmacology. Life Sciences. Februarty 2014. Pages 20-26. Rusyniak, Dan. Tox and Hound: Illbutrin. EMCRIT. April 2018.
0 Comments
Leave a Reply. |
ABOUT USVegasFOAM is dedicated to sharing cutting edge learning with anyone, anywhere, anytime. We hope to inspire discussion, challenge dogma, and keep readers up to date on the latest in emergency medicine. This site is managed by the residents of Las Vegas’ Emergency Medicine Residency program and we are committed to promoting the FOAMed movement. Archives
June 2022
Categories |
CONTACT US901 Rancho Lane, Ste 135 Las Vegas, NV 89106 P: (702) 383-7885 F: (702) 366-8545 |
ABOUT US |
WHO WE ARE |
WHAT WE DO |
STUDENTS |
RESEARCH |
FOAM BLOG |
© COPYRIGHT 2015. ALL RIGHTS RESERVED.
LasVegasEMR.com is neither owned nor operated by the Kirk Kerkorian School or Medicine at UNLV . It is financed and managed independently by a group of emergency physicians. This website is not supported financially, technically, or otherwise by UNLVSOM nor by any other governmental entity. The affiliation with Kirk Kekorian School of Medicine at UNLV logo does not imply endorsement or approval of the content contained on these pages.
Icons made by Pixel perfect from www.flaticon.com
Icons made by Pixel perfect from www.flaticon.com

 RSS Feed
RSS Feed
