|
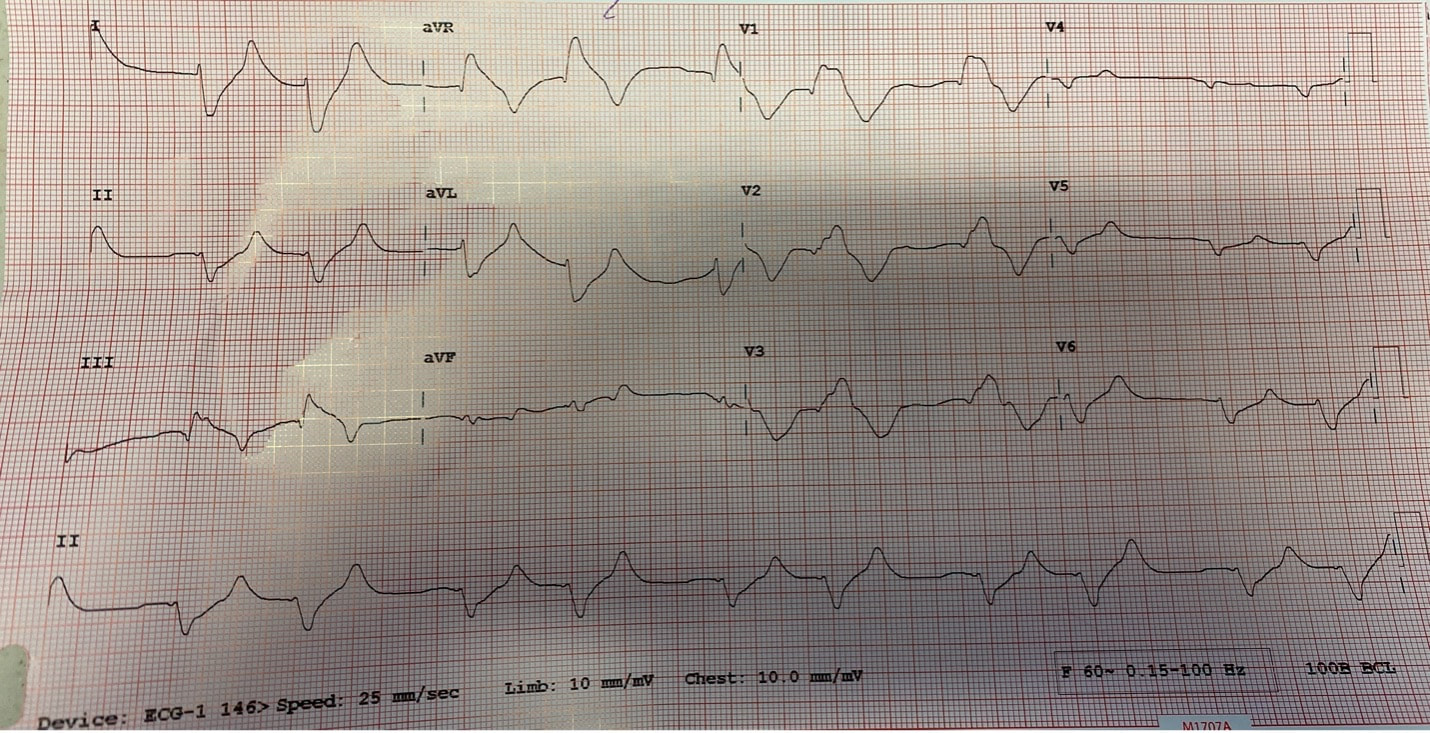
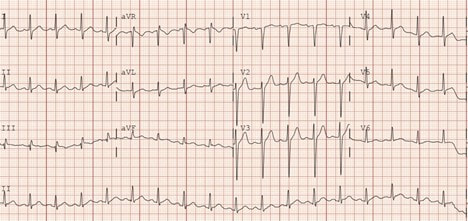
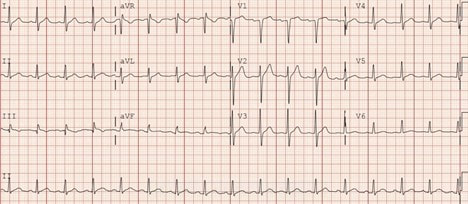
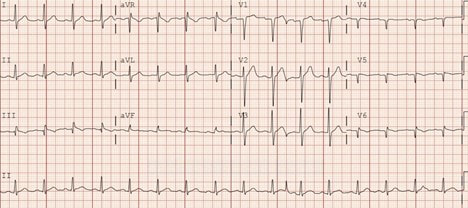
By: Chase Hamilton, PGY3 Reviewed by: David Slattery, MD Acute ST-elevation myocardial infarction is a “must-not-miss” in the world of medicine. Time is myocardium. Along with that adage is the importance of early detection and prevention of myocardial injury and potential infarction. Electrocardiograms (ECGs) are not highly sensitive in detecting early signs of potential ischemia. Also, ECG reading and interpretation is physician dependent and based on experience and education. These two factors make it difficult to reliably detect potential signs of early myocardial damage without infarction or ischemia. The morphology of the T wave in V1 can be a herring for early left anterior descending (LAD) artery disease in patients with active symptoms. The normal morphology of the T wave in V1 is inverted or flat. An upright T wave with active chest pain should make the physician more seriously consider cardiac etiology and further evaluate and study the ECG and/or ensure serial ECGs are performed2. The upright T wave is considered a type of hyperacute T wave. Specifically, it should be considered hyperacute if the T wave in V1 is larger than the T wave in V6. This is described as loss of precordial T wave balance by Marriott et al. Literature has found that it was present in 36% of subtle LAD occlusion versus 16% of precordial early repolarization1,3. A 61-year-old male presented to our Emergency Department (ED) with active chest pain. He has a history of hypertension, hyperlipidemia, and type II diabetes. He was walking down a hallway into work when the pain began just 30 minutes prior to his arrival to the ED. It was described as central and pressure-like radiated into his left jaw and arm. He felt lightheaded and sweaty. He denies nausea, abdominal pain, or ripping/tearing pain to his back. He denies alcohol or drug use but quit smoking 3 months ago. He denied any cardiac history. An EKG at time zero was obtained: This ECG shows an upright T-wave in V1 that is not necessarily more prominent that V6. It otherwise does not show any acute signs of ischemia. The patient continued to have symptoms and appeared diaphoretic. A second ECG was obtained 11 minutes later: We now see more prominence of V1 compared to V6, although subtle. We also see a new Q-wave in lead III. With active symptoms a 3rd ECG was obtained 29 minutes later: Here we see definitive prominence of an upright T wave in V1 compared with the T wave in V6. This is considered a hyperacute T wave. We also see a Q-wave in lead III and now in aVF. The morphology of the T waves in V1 through V3 are also less concave, giving further concern for cardiac pathology. At this point, a troponin had resulted within normal limits, however, the patient continued to have symptoms and a 4th ECG was obtained 5 minutes later: We now see definitive prominence of the upright T wave in V1 with an inversion of the V6 T wave. The RS complex in V4-V6 is now simply Q waves along with the Q waves in III and aVF. At this point cardiology was contacted and evaluated the patient. They were agreeable that cardiac catheterization was indicated. The patient was found to have a 95% LAD occlusion and 90% right circumflex artery (RCA) occlusion both of which were revascularized with stenting.
0 Comments
Leave a Reply. |
ABOUT USVegasFOAM is dedicated to sharing cutting edge learning with anyone, anywhere, anytime. We hope to inspire discussion, challenge dogma, and keep readers up to date on the latest in emergency medicine. This site is managed by the residents of Las Vegas’ Emergency Medicine Residency program and we are committed to promoting the FOAMed movement. Archives
June 2022
Categories |
CONTACT US901 Rancho Lane, Ste 135 Las Vegas, NV 89106 P: (702) 383-7885 F: (702) 366-8545 |
ABOUT US |
WHO WE ARE |
WHAT WE DO |
STUDENTS |
RESEARCH |
FOAM BLOG |
© COPYRIGHT 2015. ALL RIGHTS RESERVED.
LasVegasEMR.com is neither owned nor operated by the Kirk Kerkorian School or Medicine at UNLV . It is financed and managed independently by a group of emergency physicians. This website is not supported financially, technically, or otherwise by UNLVSOM nor by any other governmental entity. The affiliation with Kirk Kekorian School of Medicine at UNLV logo does not imply endorsement or approval of the content contained on these pages.
Icons made by Pixel perfect from www.flaticon.com
Icons made by Pixel perfect from www.flaticon.com

 RSS Feed
RSS Feed
